10. Central Nervous System Disorders
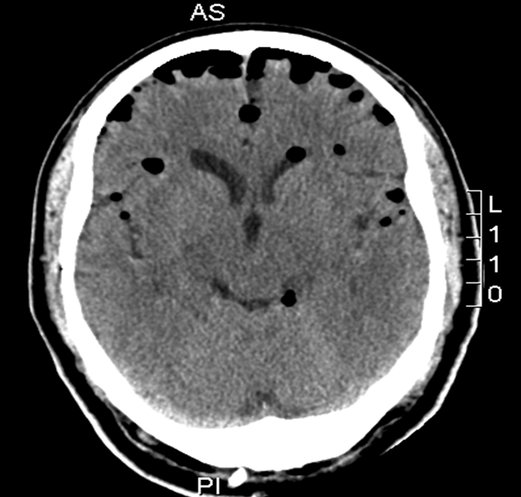
CT scan of patient with intracranial air. Patients with intracraniel air are not accepted on commercial flights because the lower cabin pressure at cruising altitude will result in the expansion of the trapped air.
Photo: Dept. of Radiology,
Rigshospitalet
General
The main aeromedical problems associated with this group of disorders all arise from conditions involving increased intracranial pressure (whether due to infarct, haemorrhage, trauma, tumour, or infection) and disorders with intracranial air.
Patients may not travel by commercial flight with increased intracranial pressure or intracranial air.
Concerning disorders with increased intracranial pressure (ICP)
Flying at normal cruising altitude with the cabin pressure at ¾ atm will aggravate the effect of increased ICP with risk of incarceration (brainstem compression). In cases where increased intracranial pressure is suspected (headache, vomiting, confusion, low pulse and high blood pressure, etc.), a CT or MR scan should be carried out, partly to establish the nature of the complaint, and partly the degree of oedema and degree of midline shift, and thereby give an indication of increased ICP.
Concerning disorders with intracranial air
A CT scan is excellent at revealing intracranial air, which can be seen after serious head trauma with fracture or after craniotomy. If the amount of intracranial air is not at a minimal level, the patient will not be able to travel by commercial flight. The reason being that while the aircraft climbs, the cabin pressure will be reduced, and the intracranial air will expand and press on the surrounding cerebral tissues.
Air transport of patients with increased ICP or intracranial air.
If such a patient, because of a lack of onsite treatment facilities, must be transported by air, it must be with an air ambulance, flying with the cabin pressure at 1 atm (sea-level flight). Patients with increased ICP must be placed in the aircraft with their head towards the nose of the plane, as the effect of the aircraft’s power is stronger at take-off than at landing. Furthermore, the bedhead should be elevated 30°.
If there are signs of seriously increased ICP, the patient can be treated with IV hypertonic sodium chloride (1 meq/ml, 50-100 ml) or Mannitol 20%, which will reduce the ICP for some hours. The patient must be escorted by an anaesthetist and anaesthetic nurse.
Air transport of patients with other neurological conditions.
Patients with neurological conditions (myopathies, cervical myelopathy decompensated myasthenia gravis, ALS, polio seqv. Parkinson’s disease, etc.) that cause limited muscle power need different types of assistance such as an escort, a wheelchair at the airport, oxygen during the flight, NIV (non-invasive ventilation), a ventilator, etc.
Stroke
About 85% of strokes consist of cerebral infarctions, 10% of intracerebral haemorrhages, and 5% of subarachnoid haemorrhages.
Cerebral infarction
Patients with infarcts, where all the neurological symptoms have disappeared quickly, will normally be accepted on a commercial flight after 4-7 days, seated and unescorted. Airline companies may differ regarding the conditions for accepting these patients.
Patients who continue to have neurological symptoms and signs, such as hemiparesis, will normally be accepted on commercial flights after 7-10 days, if there are no signs of increased ICP and the patient’s condition is good and stable. A CT or MR scan should be done to confirm the localisation and size of the infarct. Serious infarct oedema in cases of cerebral or cerebellar infarction will normally subside within 6-7 days. All patients who have had a cerebral infarct should immediately start prophylactic treatment with aspirin (ASA) 75-150 mg/day or clopidogrel 75 mg/day. Clopidogrel requires loading with 300 mg.
The patients should also receive 24-48 hours of EKG monitoring to reveal intermittent AF. Patients who have intermittent or manifest AF should start oral anticoagulation 48 hours after the infarct, later if the infract is large.
For patients with persistent neurological symptoms, the method of transportation depends entirely upon their clinical condition. Patients with severe paresis may need stretcher transport. Patients who have problems swallowing should have a gastric tube. Air ambulance transportation with accompanying anaesthetist and anaesthetic nurse may also be necessary if the patient is respiratory insufficient or unstable after the observation period.
Intracerebral hemorrhage (ICH)
Intracerebral bleeding (ICH) will always be visible on a CT scan. A distinction is made between profound basal ganglion bleeding (often related to hypertension), lobe hemorrhage and bleeding in the brain stem and cerebellum, respectively. Particularly, the profound bleeding can cause breakthrough to the ventricular system leading to significant risk of hydrocephalus and possibly increased ICP. Clinically the same hemiform deficit is seen as in the ischemic stroke. Depending on the size of the bleeding, increased ICP may occur. A new hemorrhage and hematoma expansion occur especially within the first 6 hours.
The effect of surgical evacuation of hematomas is generally questionable except from cerebellar hematomas > 3cm and subcortical hematomas < 1cm from the surface with mass effect causing clinical worsening. Treatment of patients with ICH consists of BP control with max. systolic pressure 140-150 mm Hg and mean arterial pressure (MAP)< 110 mm Hg, correction of possible bleeding disorder and in cases of hydrocephalus, possible CSF-drainage
The transport mode and escort depend entirely on the patient's neurological status. In principle you should await normalisation of any increased ICP, control of possible hydrocephalus and air resorption after possible craniotomy before flying. CSF shunting does not contraindicate flight.
Subarachnoid haemorrhage (SAH)
If the case is not hopeless, a patient with a recent subarachnoid haemorrhage should have the aneurysm closed within the first couple of days with an endovascular procedure or an operation. Today most aneurysms will be treated with endovascular coiling and fewer with craniotomy and clamping of the aneurysm. If reasonable treatment facilities are available at the location where trauma occurred, the patient should be examined and operated there.
If reasonable treatment facilities are not available locally, repatriation should be undertaken by air ambulance and the patient should be escorted by an anaesthetist and an anaesthetic nurse. If the initial bleeding is minimal, a case can be made for flying the patient at normal cruising altitude (with cabin pressure at ¾ atm), but if there are signs of increased ICP, the aircraft must fly at an altitude where the cabin pressure can be maintained at 1 atm (sea-level flight).
Even if the patient initially is not clinically affected, problems may come later. 5-14 days after a SAH the patient can get vascular spasms with risk of infarcts and general neurologic worsening including coma and death. Therefore, all SAH patients should be treated with medicine against the spasms (e.g. Nimodipine 60mg x 5 per day for 3 weeks).
In those cases where thorough and, perhaps, repeated examinations by CT or MR scan and arteriography reveal no source of bleeding, then the risk of a new bleed is small and the prognosis considerably better. These patients may, as a rule, be transported in a reclining position by commercial flight, accompanied by a physician after approximately 14 days, or, in some cases, they may travel unescorted in the seated position after achieving full mobilisation without symptoms, normally after another week.
When the patient is being moved to treatment, consultation with the relevant neurosurgical department is recommended in order to ensure unanimity as concerns the indication of surgery and transportation criteria, etc.
Transient Ischemia Attack (TIA)
All patients who have had a TIA should immediately (after a CT that excludes haemorrhage) start prophylactic treatment (see above). Be aware that the term TIA is often used incorrectly in cases with unaccountable, unspecific, and transient symptoms. The TIA diagnosis should, however, be reserved for cases with transient hemiforme (half-sided) deficits without loss of consciousness. Per definition, the attack can last for 24 hours, but usually it lasts less than 30 minutes.
All patients who have had TIA – not only those who have suffered several TIA’s – have a risk of developing new emboli. Before flying, it is recommended that these patients, besides the prophylactic treatment, should have as a minimum a CT scan or, if possible, a MR scan with diffusion-weighted images (DWI) and a Doppler ultrasound scan of the carotid arteries. Furthermore, an ECG monitoring should rule out atrial fibrillation. After a single TIA with rapid and complete remission within 24 hours and where the scan has shown no infarct or bleeding, the patient will normally be accepted unescorted on a commercial flight after a few days.
Epilepsy
In general, a patient with epilepsy should receive optimal treatment and have the medication well-adjusted before air travel. The stress related to waiting time at airports, lack of sleep, the changing of time zones, etc., can increase the risk of an attack. Using a supplementary benzodiazepine from the day before travelling to the day after arrival as prevention against attack is recommended in some patients for long journeys, especially with different time zones.
An epilepsy patient who has suffered an attack will normally be accepted on a commercial flight 24 hours after the event.
Cases of frequent or several attacks must be evaluated individually.
If a patient has recently been diagnosed with epilepsy (and other neurological disorders have been excluded), the airline companies often demand a physician as an escort.
Sleep apnoea
Patients with moderate to severe sleep apnoea may bring their CPAP machine in the cabin if agreed to by the airline company.
Intracranial infections
Patients suffering from intracranial infections may be transported by commercial flight when normal ICP has been assured, that they are no longer a source of infection, and their circulation and respiration are stable. This applies both for patients with meningitis, encephalitis, or a brain abscess. Disposition and escort are subject to the clinical condition of the patient.
In case of a lack of local treatment facilities, a patient with intracranial infection and increased ICP will need to be evacuated by air ambulance, maintaining sea-level cabin pressure.
Intracranial tumours and hydrocephalus
Both intracerebral and extracerebral intracranial tumours, especially when malignant, can cause a rapid development of increased ICP. This is partly due to the growth itself and partly to oedema in the tumour’s surroundings or a blockade of the ventricle, causing hydrocephalus. If the tumour first makes its appearance during an overseas trip, the patient is at risk of being “trapped”, because the increased ICP will result in commercial airlines refusing to transport him or her.
Nevertheless, the oedema surrounding the tumour can be reduced by the administration of high doses of steroids (for example, prednisolone 150 mg/day) for a short period. If this normalises the ICP and the patient can be accepted on a commercial flight, it is important that the patient travel back immediately before the ICP rises again.
Before travelling by air, patients with hydrocephalus need a ventricular drainage.
Head injury
Concussion
In cases of mild concussion, there is rarely cerebral oedema, therefore these patients may travel by air as normal passengers on commercial flights as soon as they are mobile without symptoms, usually within 1-2 days.
In cases of more severe concussion with loss of consciousness more than 3-5 min., it is necessary to do a CT scan to exclude intracranial damage. Concussions with accompanying oedema may be subject to increased ICP for several days. Travel by commercial flight must be delayed until the patient is without signs of increased ICP and is fully mobilised without symptoms. The patient will then normally be able to travel, seated and unescorted.
Skull fractures
Non-dislocated skull fractures do not give rise to problems. Only attendant lesions of the brain (contusions or hematoma) or dura will lead to restrictions by commercial flights. Fractures accompanied by the tearing of the dura, with the loss of spinal fluid through the nose, pharynx, or ear and eventually with intracranial air, present a serious aeromedical problem. Such a defect will always be a gateway for infection. There will be a strong outward flow of cerebrospinal fluid during ascent due to the change in cabin pressure, and, during descent, it is even possible for air together with blood/secretion to be sucked in through the nasal fossae or the middle ear if the original fracture involves these areas.
If loss of spinal fluid does not stop spontaneously within 1-2 weeks, the patient should be operated on to close the defect. A patient suffering from a dural lesion with loss of spinal fluid will not be accepted on commercial flights. Should transportation be unavoidable, e.g. because of the lack of treatment facilities, this must be undertaken by air ambulance maintaining sea-level pressure in the cabin.
A patient with a non-dislocated cranial fracture should be placed under observation for a few days before flying in order to ensure that there are no attendant cerebral injuries or dural lesions. If the patient, hereafter, is mobilised without symptoms, the journey can be made, seated and unescorted, by commercial flight.
Epidural hematoma
An epidural hematoma after a cranium trauma is almost always associated with a fracture in the cranium. As bleeding may develop insidiously over 24 hours, so CT scan and a 24-hour observation period after a cranium trauma are important. Most epidural hematomas greater than 30 ml are operated acute by craniotomy with evacuation of hematoma and hemostasis assurance. Minor hematomas can be treated without operation but controlled with CT scan.
Transport: see Craniotomy.
Subdural hematoma
Most patients with significant subdural hematomas are operated. The hematoma is evacuated, and drains are inserted for 1-2 days. Minor subdural hematoma that do not produce pressure symptoms can be treated without surgery. They should be controlled with CT scan until resorption. When CT scan has confirmed that the subdural hematoma no longer causes pressure on underlying structures, the patients are allowed to fly.
Transport after surgery: see Craniotomy.
Craniotomy
After a brain operation, there will almost always be oedema and smaller air pockets that will gradually be resorbed over days to weeks.
Transport: A patient is first accepted on commercial flights when there is no significant air or oedema in the brain. Patients who at this time have no neurological symptoms will usually be able to travel by air, sitting and unaccompanied. For patients with neurological symptoms, transport and escorting must be assessed according to the clinical condition. Prevention of seizures with antiepileptics should be considered.
Lumbar puncture
After a lumbar puncture, the patient can in principal fly just after the puncture. Patients who develop a headache due to a lumbar puncture need to wait until the symptoms disappear before flying, possibly after a blood patch.
001. Frontpage
001. Foreword
001. Contributors
001. Aeromedical Problems
012. Planning the Air Transportation of Patients
013. Airline Requirements
015. Transportation of Disabled Persons
016. Cardiac Disorders
019. Gastrointestinal Disorders
010. Central Nervous System Disorders
011. Ear, Nose, and Throat Disorders
012. Eye Disorders
013. Mental Disorders
014. Gynaecological and Pregnancy Problems
015. Transportation of Sick Children
016. Infectious Diseases
017. Orthopaedic Injuries
018. Cancer
120. Acute Mountain and Decompression Sickness
021. Burns and Plastic Surgical Problems
122. Airsickness
123. Jet Lag
124. The STEP System
125. Specialised Transportation of Patients
126. First Aid on Board – Legal Considerations
27. The History of Air Transportation of Patients
28. Oxygen supplementation in flight - a summary
Latest update: 29 - 02 - 2020